Burkina Faso has an estimated population of 24.1 million as of mid-2025. With a GDP per capita of approximately $874 USD, the nation faces ongoing development challenges but continues to make progress in health outcomes. Life expectancy stands at 63.9 years overall, 64.8 years for females, and 62.96 years for males. The infant mortality rate remains high at approximately 44.8 deaths per 1,000 live births, signaling persistent gaps in neonatal care.
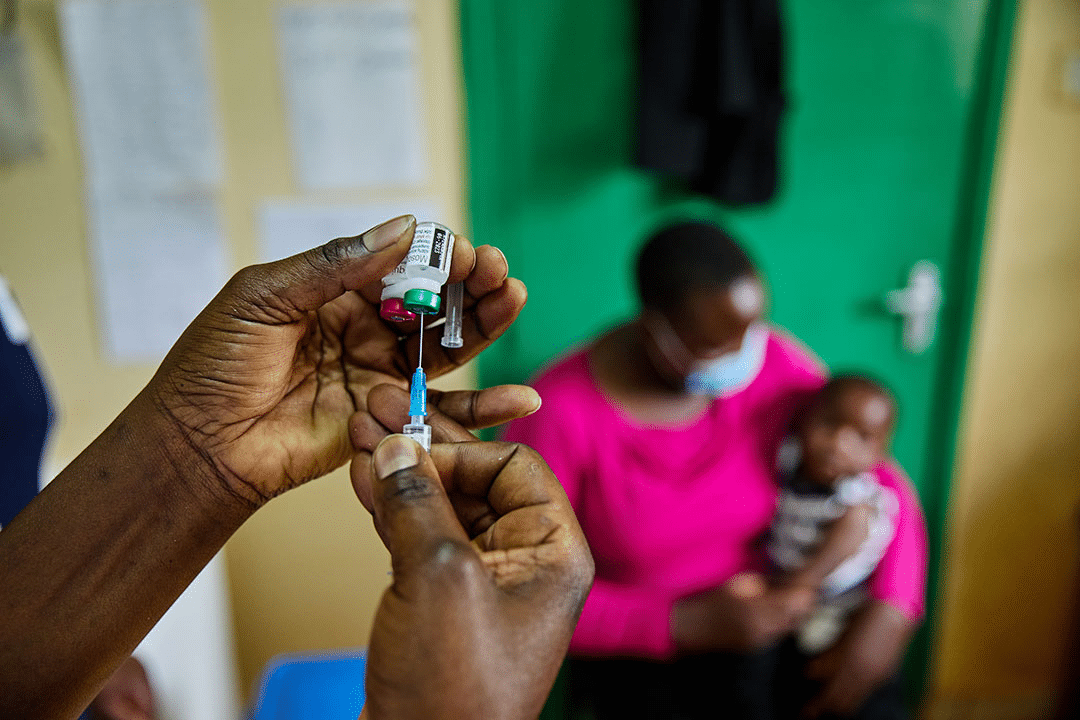
Maternal, Newborn & Child Health
Burkina Faso has achieved notable improvements in maternal and child health. The maternal mortality ratio declined to an estimated 263.8 deaths per 100,000 live births, reflecting increased institutional deliveries and investment in maternal health services. The under-five mortality rate fell to 48 deaths per 1,000 live births as of 2021. However, significant disparities remain between urban and rural areas, where access to skilled birth attendants, emergency obstetric care, and newborn services is still limited. Continued efforts are needed to expand universal health coverage and reduce geographic and socioeconomic barriers to care.

Malaria, Tuberculosis (TB), and Neglected Tropical Diseases (NTDs)
Malaria remains one of Burkina Faso’s most urgent public health concerns, accounting for 43% of consultations, over 60% of hospitalizations, and 30% of deaths in the country every year. In 2022, the country reported approximately 8 million cases and over 16,600 malaria-related deaths, among the highest in the region. Tuberculosis incidence remains elevated at 134 cases per 100,000 population in 2023, driven by limited access to diagnostics, treatment interruptions, and co-infection with HIV. The country is also endemic for all five major preventable chemotherapy-neglected tropical diseases (PC-NTDs): lymphatic filariasis, onchocerciasis, schistosomiasis, soil-transmitted helminthiasis, and trachoma, all of which disproportionately affect the most marginalized populations and can lead to chronic disability and stigma if untreated.
Disease Surveillance, Emergency Preparedness & Outbreak Response
Burkina Faso frequently experiences recurrent disease outbreaks, including cholera, COVID-19, polio, monkeypox, and measles. The country has made meaningful investments in the Integrated Disease Surveillance and Response (IDSR) framework and participates in regional health security initiatives. However, its ability to detect, report, and respond to health emergencies is constrained by under-resourced laboratories, limited public health infrastructure, and conflict-related displacement in certain regions. Continued support is essential to strengthen real-time data collection, emergency logistics, and interagency coordination.

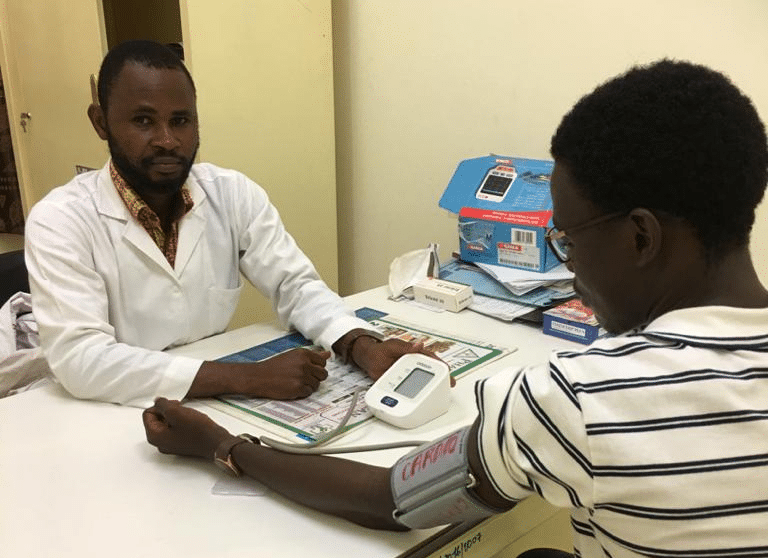
Non-Communicable Diseases (NCDs)
Non-communicable diseases are a rapidly emerging health burden in Burkina Faso. According to WHO data, NCDs accounted for 34.8% of all deaths in the country in 2019, with projections indicating a continued upward trend. Cardiovascular diseases, diabetes, cancers, and chronic respiratory conditions are becoming more prevalent due to urbanization, changes in dietary patterns, physical inactivity, and tobacco use. The country currently lacks a national NCD strategy, and access to early diagnosis and long-term management remains limited. Integrated NCD screening, health promotion, and primary care-based interventions are urgently needed.
Our Projects & Programmes
Maternal, Newborn, and Child Health Capacity Building
We implement comprehensive training programs that enhance the capabilities of CHWs. These frontline health agents are equipped to deliver vital MNCH services, including antenatal education, birth preparedness, and postnatal follow-ups, thereby closing the gap between formal health systems and remote communities.
Community Interventions for Tuberculosis Prevention and Treatment
Our TB-focused community interventions aim to increase awareness, reduce stigma, and boost treatment adherence. Through educational campaigns, community mobilization, and collaboration with local leaders, we address barriers to TB diagnosis and support patients throughout their treatment journey.
Training CHWs for Malaria Diagnosis and Treatment
We train CHWs to conduct rapid diagnostic testing and administer appropriate first-line antimalarial medications. These efforts help detect malaria early, reduce complications, and expand access to life-saving treatment in high-burden regions.
Monitoring and Evaluation
We develop and implement robust M&E frameworks to track the effectiveness, reach, and impact of all health initiatives. Routine data collection, community feedback, and midline and endline evaluations ensure that interventions remain adaptive and aligned with local health priorities.